Integrative Therapies for Insomnia & Stress and Adjunctive Therapies for Anxiety & Depression
I help people with insomnia, stress, anxiety and depression using natural, evidence-based treatments to alleviate the biological causes contributing to these conditions, including gold-standard, drug-free treatment of insomnia. My insomnia program includes a stress management component designed to not only reduce stress but also optimize health and well-being.
The insomnia program is designed to help patients become good sleepers for the rest of their lives as well as to maximize resilience to stress by providing tools to help reduce the release of stress hormones and defuse stressed thinking patterns.
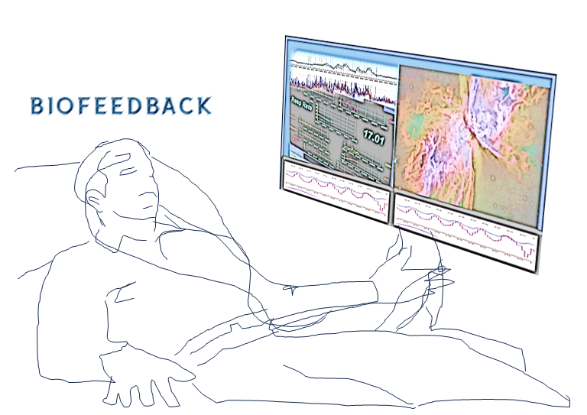
The base program is 12 sessions, which includes the stress-resilience component as well as a free biofeedback assessment to determine which relaxation techniques work best for you. For patients who grapple with anxiety that leaves them staring at the ceiling at night, the program offers an anxiety component of 3 additional sessions using adjunctive, evidence-based therapies for a total of 15 sessions.
I believe that spending the time to make my patients more stress resilient will further optimize sleep, physical health and mental well-being. That’s why I incentivize completing the base program by offering the option of additional free sessions including two biofeedback-assisted relaxation training sessions, one hypnosis for relaxation session, a sleep-environment assessment session, as well as a diet & exercise counseling session to optimize sleep health. Patients who complete the base program can get up to 17 sessions for the price of 11. Those who also complete the anxiety component also get the option of the additional free sessions for a total of up to 20 sessions for the price of 14.
Anxiety and depression are biological bedfellows of sleep problems with any one triggering the others. Mood Change Medicine offers CBT-I, the gold-standard treatment for insomnia. Our CBT-I program also includes light therapy for normalizing circadian rhythms and biofeedback for relaxation.
Mood Change Medicine’s integrative approach to mental health uses evidence-based therapies as adjuncts to support the work your doing with your psychotherapist. Our integrative approaches address the biological components of anxiety and depression, such as insufficient, non-restorative sleep, disrupted circadian and interpersonal rhythms, out-of-control psychophysiological stress, soaring neuroinflammation and plummeting neuroplasticity.
WHY USE AN INTEGRATIVE APPROACH ?

Sleeplessness, stress, anxiety and depression are not exclusively mental processes. These states initiate and coalesce in the body as well as in the mind. That’s why optimal treatment for insomnia, stress, anxiety and depression addresses both mind and body.
Circadian disruption and other biological triggers like changes in brain biochemistry play a large role in insomnia.
Because depression and anxiety cause our minds to inhabit a hamster wheel of depressed and anxious thoughts incessantly replaying like a mantra of misery and apprehension, it makes us feel that these emotional states are solely caused by social, situational or purely psychological factors. It seems as though if only we could master our minds or gain control over our problems, we could hit the pause button and make these life-disrupting feelings end. But, the fact is, anxiety and depression are not purely mental constructions or the results of inability to find solutions to life challenges.
Anxiety and depression also live in our bodies, and what goes on in the body permeates into the mind.
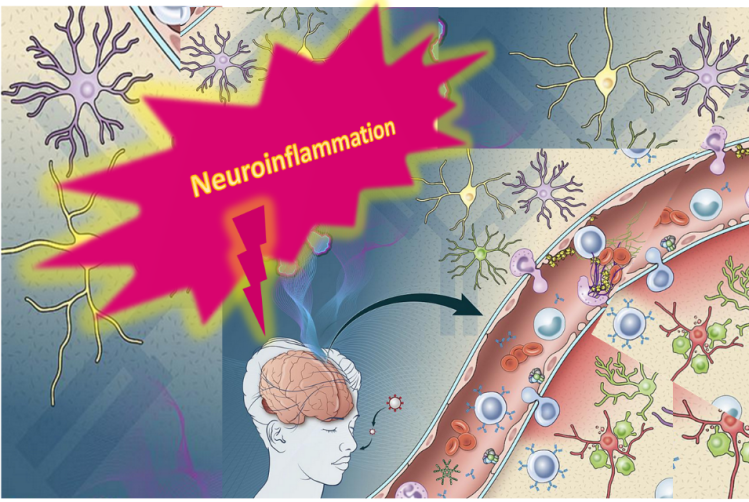
Neuroinflammation has been implicated as an important part of the mechanism driving anxiety and depression. 1, 2, 3, 4
Life stressors like fights in the family, financial problems or intimidating social interactions can trigger anxiety. The resultant anxiety leads to physical changes that feeds on itself, creating more anxiety. If this vicious cycle of anxiety goes on too long, our biochemistry becomes fertilizer for depression.
Anxiety and depression spring from the same biochemical well and are part of a vicious cycle of stressed thinking fueling stressed physiology which, in turn, further fuels stressed thinking.
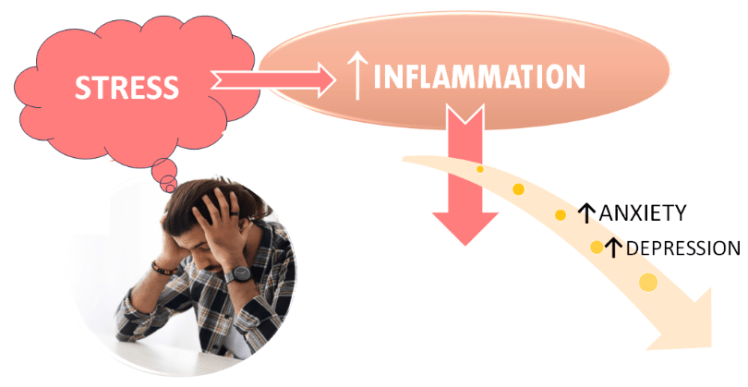
Stress is the common thread tying insomnia, circadian disruption, anxiety and depression together. Stress spikes ignite a firestorm of inflammation suppressing sleep hormone melatonin production in the pineal gland. Melatonin is one of the bodie’s key inflammation fighters.
The biochemistry created by this hamster wheel of emotions can alter our circadian rhythms and trigger insomnia, which adds fuel to the vicious cycle in which all three conditions are intertwined. Lifestyle factors that negatively impact the biochemistry of anxiety, depression and insomnia add more fuel. By simultaneously addressing the biochemistry while also targeting problematic thinking patterns, we send our minds a biochemical message that leads to positive changes in mood and thinking.
Talk-therapy with your psychotherapist, combined with Mood Change Medicine’s evidence-based treatments that target the biology of these conditions, can break vicious cycles driven by both the mental and physical causes of anxiety, depression and insomnia.
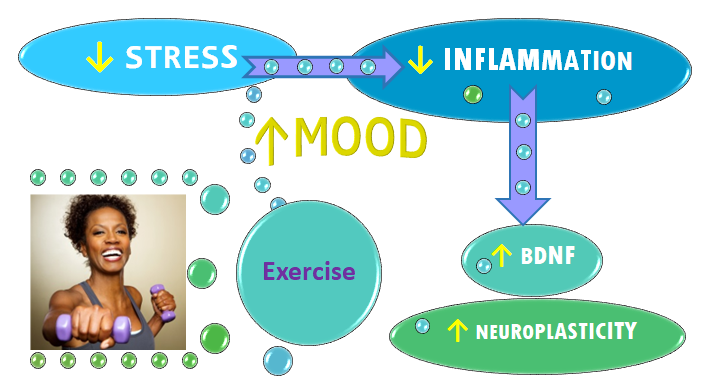
An array of tools encompassing this integrative, mind-body strategy are used to enhance the efficacy of standard talk therapies. Mood Change Medicine tools include cognitive behavioral therapy for insomnia (CBT-I) to improve sleep, biofeedback to defeat psychophysiological stress and neuroinflammation; hypnosis to harness the power of the subconscious and help change undesirable habits, exercise prescription to reduce stress and boost neuroplasticity, and diet therapy for optimizing mood.
Mood Change Medicine’s Tool box of time-tested techniques includes:
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Transdiagnostic Sleep & Circadian Intervention (TranS-C)
- Biofeedback-Assisted Relaxation Therapy (BART)
- Hypnotherapy
- Polyvagal-informed therapy
- Motivational Interviewing
- Light Therapy
- Diet and Nutrient Therapy
- Exercise Prescription
- Mindfulness-Based Stress Reduction (MBSR)
Biofeedback is part of sleep treatment programs at prestigious health care systems like Mayo Clinic in their sleep program “Insomnia treatment: Cognitive behavioral therapy instead of sleeping pills”. The Cleveland Clinic also uses biofeedback in their CBT-I program for the sleep anxiety that often accompanies insomnia.
Exposure to low levels of light, depression and insomnia can reduce melatonin levels and disrupt its circadian rhythm, which light therapy can help to restore. 5, 6 Light therapy is far more effective than melatonin supplementation alone. 7, 8, 9, 10, 11, 12, 13
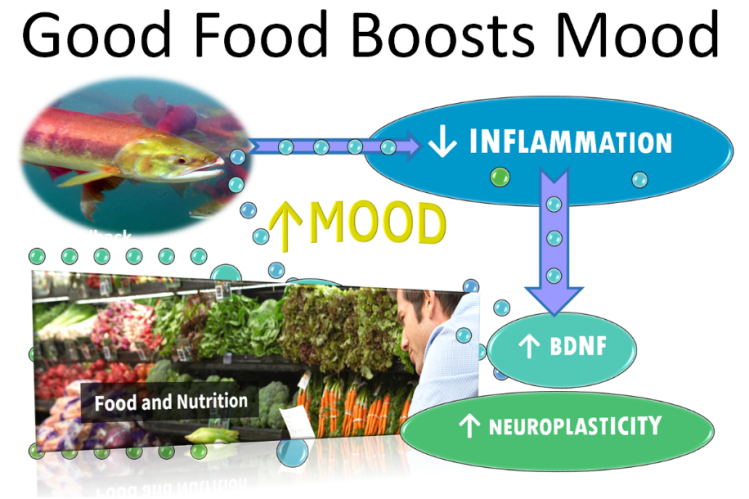
Mood Change Medicine offers adjunctive dietary recommendations that address common biological drivers of anxiety and depression such as thyroid dysfunction, which accounts for up to 45% of depression cases and 30% of anxiety, according to a 2018 study in the journal JAMA Psychiatry. 14 Researchers point to the strong association between the Western diet also known as Standard American Diet (SAD) and the risk for depression and anxiety.15 Mood Change Medicine provides support for making positive changes in your diet.
Stress-induced neuroinflammation and disrupted neuroplasticity are biological drivers of anxiety and depression. Mood Change Medicine helps reverse stress and its physiological costs using biofeedback and hypnosis to shift the mind and body into a more relaxed state. Mood Change Medicine uses proven behavior-change methods to help people make lifestyle changes that reduce neuroinflammation and boost neuroplasticity. We also offer an individualized, anti-inflammatory diet & exercise program for those wanting to further optimize their well-being.
Inflammation causes a drop in a neurochemical called Brain-derived neurotrophic factor (BDNF) and in neuroplasticity—the brain’s resiliency network. When BDNF and neuroplasticity are operating properly, they repair such inflammatory damage and depression remits. When depression is raging, BDNF plummets. When depression wanes, BDNF levels rise.
Researchers report that in other countries “lifestyle management is recommended as the first-line treatment approach” for mental health conditions including depression and anxiety. A meta-analysis that pooled data from numerous studies found that all forms of exercise improved mental health. “Physical activity should be a mainstay approach in the management of depression, anxiety and psychological distress,” the researchers concluded. 16
By embarking upon the journey in a way that prioritizes what feels most compelling and attainable—one-step-at-a-time, in manageable, bite-sized chunks—we make the pathway out of sleeplessness, angst and anguish more relaxed, intuitive, spontaneous and hopeful.
Mood Change Medicine offers integrative treatment of insomnia and stress and adjunctive therapies that address the biological drivers of anxiety and depression.
Find out more about our services:
Mood Change Medicine’s Integrative Approach to Insomnia
Mood Change Medicine’s Integrative Approach to Stress & Anxiety
Mood Change Medicine’s Integrative Approach to Depression
Care informed by the understanding that emotional and physical wellbeing are deeply connected
The website’s Mood Change Library page contains health related articles on topics of interest to the general public and as well as medical professionals. Mood Change Library
Citations
- Cowen PJ, Browning M. “What has serotonin to do with depression?” World Psychiatry. 2015 Jun;14(2):158-60. doi: 10.1002/wps.20229. PMID: 26043325; PMCID: PMC4471964. ↩︎
- Berk M, Williams LJ, Jacka FN, O’Neil A, et al. “So depression is an inflammatory disease, but where does the inflammation come from?” BMC Med. 2013 Sep 12;11:200. doi: 10.1186/1741-7015-11-200. PMID: 24228900; PMCID: PMC3846682. ↩︎
- Pitsavos C, Panagiotakos DB, Papageorgiou C, Tsetsekou E, Soldatos C, Stefanadis C. “Anxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA study.” Atherosclerosis. 2006 Apr;185(2):320-6. doi: 10.1016/j.atherosclerosis.2005.06.001. Epub 2005 Jul 11. PMID: 16005881 ↩︎
- Hu P, Lu Y, Pan BX, Zhang WH. “New Insights into the Pivotal Role of the Amygdala in Inflammation-Related Depression and Anxiety Disorder.” Int J Mol Sci. 2022 Sep 21;23(19):11076. doi: 10.3390/ijms231911076. PMID: 36232376; PMCID: PMC9570160. ↩︎
- von Bahr C, Ursing C, Yasui N, et al. “Fluvoxamine but not citalopram increases serum melatonin in healthy subjects – an indication that cytochrome P450 CYP1A2 and CYP2C19 hydroxylate melatonin.” Eur J Clin Pharmacol. 2000;56:123-7. View abstract. ↩︎
- Mishima K, Okawa M, Shimizu T, Hishikawa Y. “Diminished melatonin secretion in the elderly caused by insufficient environmental illumination.” J Clin Endocrinol Metab. 2001;86:129-34. View abstract. ↩︎
- Lewy AJ, Ahmed S, Jackson JM, Sack RL. “Melatonin shifts human circadian rhythms according to a phase-response curve.” Chronobiol Int. 1992;9:380-92. View abstract. ↩︎
- Zaidan, R., Geoffriau, M., Brun, J., Taillard, J., Bureau, C., Chazot, G., and Claustrat, B. “Melatonin is able to influence its secretion in humans: description of a phase-response curve.” Neuroendocrinology. 1994;60(1):105-112. View abstract. ↩︎
- Deacon, S. and Arendt, J. “Melatonin-induced temperature suppression and its acute phase-shifting effects correlate in a dose-dependent manner in humans.” Brain Res. 8-7-1995;688(1-2):77-85. View abstract. ↩︎
- Steinlechner, S. “Melatonin as a chronobiotic: PROS and CONS.” Acta Neurobiol.Exp. (Warsz.) 1996;56(1):363-372. View abstract. ↩︎
- Hatonen, T., Alila, A., and Laakso, M. L. “Exogenous melatonin fails to counteract the light-induced phase delay of human melatonin rhythm.” Brain Res. 2-26-1996;710(1-2):125-130. View abstract. ↩︎
- Cagnacci, A., Soldani, R., and Yen, S. S. “Contemporaneous melatonin administration modifies the circadian response to nocturnal bright light stimuli.” Am J Physiol. 1997;272(2 Pt 2):R482-R486. View abstract. ↩︎
- Lewy, A. J. and Sack, R. L. Exogenous melatonin’s phase-shifting effects on the endogenous melatonin profile in sighted humans: a brief review and critique of the literature. J Biol Rhythms. 1997;12(6):588-594. View abstract. ↩︎
- Siegmann EM, Müller HHO, Luecke C, Philipsen A, Kornhuber J, Grömer TW. “Association of Depression and Anxiety Disorders With Autoimmune Thyroiditis: A Systematic Review and Meta-analysis.” JAMA Psychiatry. 2018 Jun 1;75(6):577-584. doi: 10.1001/jamapsychiatry.2018.0190. Erratum in: JAMA Psychiatry. 2019 Jun 19;: PMID: 29800939; PMCID: PMC6137529. ↩︎
- Jacka FN, Pasco JA, Mykletun A, Williams LJ, Hodge AM, O’Reilly SL, Nicholson GC, Kotowicz MA, Berk M. “Association of Western and Traditional Diets With Depression and Anxiety in Women.” Am J Psychiatry. 2010;167 (3):305–311. [PubMed] [Google Scholar] ↩︎
- Singh B, Olds T, Curtis R, Dumuid D, et al. “Effectiveness of physical activity interventions for improving depression, anxiety and distress: an overview of systematic reviews.” Br J Sports Med. 2023 Sep;57(18):1203-1209. doi: 10.1136/bjsports-2022-106195. Epub 2023 Feb 16. PMID: 36796860; PMCID: PMC10579187. ↩︎
By using this website, you agree to accept MoodChangeMedicine.com website’s terms of use, which can be viewed here.
Terms of Use







Discussion
No comments yet.